The kidneys are essential organs that filter the blood and balance fluids in the body. If they begin to work less efficiently, it can lead to renal failure. There are two types of renal failure: acute and chronic.
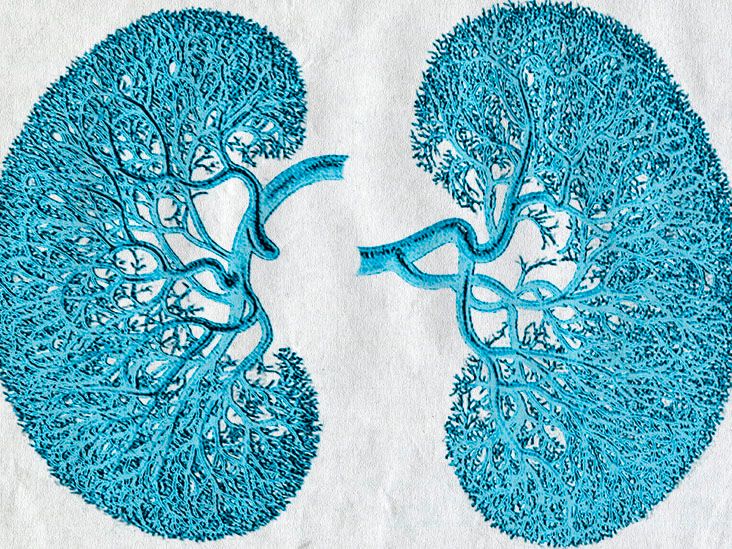
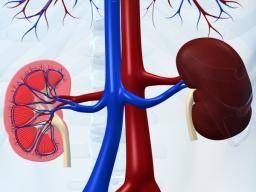
The kidneys are two bean-shaped organs on either side of the spine, just below the ribcage. They have a range of essential functions, including filtering waste products and excess substances from the bloodstream, regulating the body’s balance of fluids and electrolytes, and helping control blood pressure.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), renal failure happens if someone has less than
This article explores the different types of renal failure, including their symptoms, causes, diagnosis, and treatments for both.
Acute renal failure or acute kidney injury (AKI) refers to a sudden and often reversible loss of kidney function. The condition affects the kidneys’ ability to filter waste products, excess fluids, and electrolytes from the bloodstream.
This type of renal failure can happen suddenly, often within a few hours or days.
Doctors categorize acute renal failure into several subtypes based on its underlying causes:
- Pre-renal: A reduction in blood flow to the kidney plays a role in causing this subtype. It is the leading cause of kidney injury. Factors that reduce blood flow to the kidneys include:
- severe dehydration
- low blood pressure (hypotension)
- heart failure
- co-occurring health conditions that constrict blood vessels
- Intrinsic or renal: This subtype occurs due to direct damage to the kidney tissue. Common causes of it include:
- acute tubular necrosis (ATN), a disease that occurs due to a lack of blood supply to the kidney
- nephrotoxic substances, such as certain medications or toxins
- infections
- glomerulonephritis or inflammation of a part of the kidneys called the glomeruli
- a vascular disorder that affects blood vessels
- Post-renal: Post-renal AKI occurs when a physical obstruction prevents the flow of urine from the kidneys and to the bladder. Obstruction can occur due to:
- kidney stones
- tumors
- blockages in the urinary tract
Symptoms
The symptoms of acute renal failure can vary depending on its severity and underlying cause. Common symptoms and signs include:
- decreased urine output or an absence of urine (anuria)
- fatigue and weakness
- nausea and vomiting
- swelling or edema, particularly in the legs, ankles, or face
- shortness of breath
- high blood pressure (hypertension)
- chest pain or pressure in the chest
- irregular heart rhythms (arrhythmias)
- confusion or altered mental state
Stages
Doctors categorize acute renal failure into
- Stage 1: Early stage failure. There may be no symptoms.
- Stage 2: Oligo-anuria, meaning a person urinates less frequently. This leads to fluid retention, waste production accumulation, increased blood pressure, and potential heart failure.
- Stage 3: Kidney function slowly recovers, but there may still be a substantial loss of water and electrolytes. If this stage lasts for longer than 3 months, a person may have progressed to chronic kidney disease.
- Stage 4: Restitution or return of kidney function.
Diagnosis
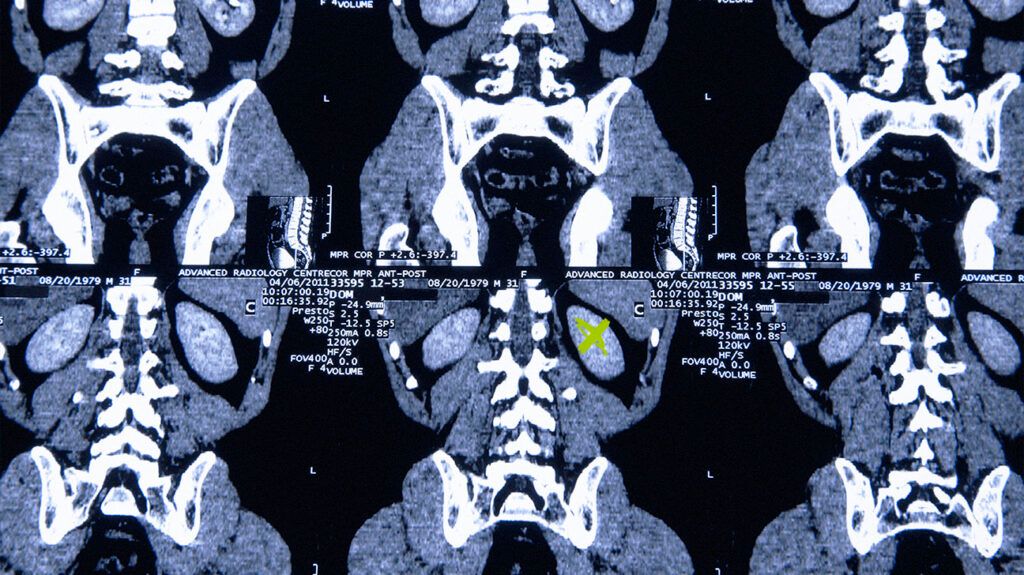
Diagnosing acute renal failure typically
- medical history review
- physical examination
- laboratory tests, including serum creatinine and blood urea nitrogen (BUN)
- imaging studies, such as ultrasound or CT scans
- urinalysis
Treatment
Treatment for acute renal failure depends on its underlying cause, severity, and stage. Standard treatment approaches
- addressing the underlying cause, such as correcting dehydration or discontinuing nephrotoxic medications
- supportive care to manage symptoms and maintain fluid and electrolyte balance
- dialysis to temporarily take over the kidneys’ filtering function until they recover
Learn more about acute renal failure.
Chronic renal failure, also known as chronic kidney disease (CKD), is a long-term and progressive decline in kidney function. Unlike acute renal failure, CKD
Causes
Common contributing factors and causes include:
- high blood pressure
- diabetes
- glomerulonephritis
- polycystic kidney disease (PKD)
- urinary tract obstructions, such as kidney stones or tumors
- certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and some antibiotics
Stages
Doctors categorize chronic renal failure into different stages based on the level of kidney function and the presence of complications:
- Stage 1 — Kidney damage with normal GFR: There is mild kidney damage in this early stage, but the glomerular filtration rate (GFR) — a measure of kidney function — remains normal.
- Stage 2 — Mildly reduced GFR: Kidney function is mildly reduced in this stage and has a slightly lower than average GFR. Some individuals may experience mild symptoms or complications.
- Stage 3 — Moderately reduced GFR: Kidney function is moderately reduced, and individuals may experience noticeable symptoms and complications.
- Stage 4 — Severely reduced GFR: In this stage, kidney function is significantly impaired, and individuals are at high risk of experiencing complications and symptoms.
- Stage 5 — End stage renal disease (ESRD): This is the most advanced stage of chronic renal failure. Kidney function is severely compromised, and individuals often require kidney replacement therapy, such as dialysis or a transplant, to sustain life.
Symptoms
Chronic renal failure may not exhibit noticeable symptoms in its early stages. As CKD progresses, individuals may experience a range of symptoms, which can
- fatigue and weakness
- nausea and vomiting
- persistent itching
- foamy or bubbly urine
- increased or decreased urination
- blood in the urine (hematuria)
- swelling in the legs, ankles, or face (edema)
- a loss of appetite
- muscle cramps
- high blood pressure
- difficulty sleeping
- cognitive changes and trouble concentrating
Diagnosis
Doctors diagnose chronic renal failure through a
Key diagnostic markers include:
- estimated glomerular filtration rate (eGFR)
- serum creatinine levels
- urine tests
Just as with acute renal failure, imaging studies are useful to assess kidney size and structure.
Treatment
Treatment for CKD aims to slow the progression of the disease, manage its symptoms, and address underlying causes. The severity of the disease can play a role in choosing the most appropriate treatment method.
Common approaches
- blood pressure management
- diabetes management, if necessary
- medications
- dialysis
- a kidney transplant
A person with CKD should also make dietary modifications to adjust their sodium, potassium, phosphorus, and protein intake.
Learn more about CKD.
There are two types of renal failure. Acute renal failure happens rapidly, often as a result of dehydration, medications, or infections. The outlook for acute renal failure tends to be favorable, as individuals have the potential to recover completely.
Conversely, chronic renal failure is more gradual kidney failure, spanning weeks or months. This form of renal failure is typically progressive, leading to long-term consequences if people do not manage it appropriately.